NovoLog for Treatment of Diabetes - Novolog Full Prescribing Information
Brand Name: NovoLog
Generic Name: insulin aspart
Dosage Form: injection
Contents:
Indications and Usage
Dosage and Administration
Dosage Forms and Strengts
Contraindications
Warnings and Precautions
Adverse Reactions
Drug Interactions
Use in Specific Populations
Overdosage
Description
Clinical Pharmacology
Nonclinical Toxicology
Clinical Studies
How Supplied / Storage and Handling
NovoLog, insulin aspart, patient information (in plain English)
Indications and Usage
Treatment of diabetes mellitus
NovoLog is an insulin analog indicated to improve glycemic control in adults and children with diabetes mellitus.
Dosage and Administration
Dosing
NovoLog is an insulin analog with an earlier onset of action than regular human insulin. The dosage of NovoLog must be individualized. NovoLog given by subcutaneous injection should generally be used in regimens with an intermediate or long-acting insulin [see Warnings and Precautions, How Supplied/Storage and Handling]. The total daily insulin requirement may vary and is usually between 0.5 to 1.0 units/kg/day. When used in a meal-related subcutaneous injection treatment regimen, 50 to 70% of total insulin requirements may be provided by NovoLog and the remainder provided by an intermediate-acting or long-acting insulin. Because of NovoLog's comparatively rapid onset and short duration of glucose lowering activity, some patients may require more basal insulin and more total insulin to prevent pre-meal hyperglycemia when using NovoLog than when using human regular insulin.
Do not use NovoLog that is viscous (thickened) or cloudy; use only if it is clear and colorless. NovoLog should not be used after the printed expiration date.
Subcutaneous Injection
NovoLog should be administered by subcutaneous injection in the abdominal region, buttocks, thigh, or upper arm. Because NovoLog has a more rapid onset and a shorter duration of activity than human regular insulin, it should be injected immediately (within 5-10 minutes) before a meal. Injection sites should be rotated within the same region to reduce the risk of lipodystrophy. As with all insulins, the duration of action of NovoLog will vary according to the dose, injection site, blood flow, temperature, and level of physical activity.
NovoLog may be diluted with Insulin Diluting Medium for NovoLog for subcutaneous injection. Diluting one part NovoLog to nine parts diluent will yield a concentration one-tenth that of NovoLog (equivalent to U-10). Diluting one part NovoLog to one part diluent will yield a concentration one-half that of NovoLog (equivalent to U-50).
Continuous Subcutaneous Insulin Infusion (CSII) by External Pump
NovoLog can also be infused subcutaneously by an external insulin pump [see Warnings and Precautions, How Supplied/Storage and Handling]. Diluted insulin should not be used in external insulin pumps. Because NovoLog has a more rapid onset and a shorter duration of activity than human regular insulin, pre-meal boluses of NovoLog should be infused immediately (within 5-10 minutes) before a meal. Infusion sites should be rotated within the same region to reduce the risk of lipodystrophy. The initial programming of the external insulin infusion pump should be based on the total daily insulin dose of the previous regimen. Although there is significant interpatient variability, approximately 50% of the total dose is usually given as meal-related boluses of NovoLog and the remainder is given as a basal infusion. Change the NovoLog in the reservoir, the infusion sets and the infusion set insertion site at least every 48 hours.
Intravenous Use
NovoLog can be administered intravenously under medical supervision for glycemic control with close monitoring of blood glucose and potassium levels to avoid hypoglycemia and hypokalemia [see Warnings and Precautions, How Supplied/Storage and Handling]. For intravenous use, NovoLog should be used at concentrations from 0.05 U/mL to 1.0 U/mL insulin aspart in infusion systems using polypropylene infusion bags. NovoLog has been shown to be stable in infusion fluids such as 0.9% sodium chloride.
Inspect NovoLog for particulate matter and discoloration prior to parenteral administration.
Dosage Forms and Strengts
NovoLog is available in the following package sizes: each presentation contains 100 units of insulin aspart per mL (U-100).
- 10 mL vials
- 3 mL PenFill cartridges for the 3 mL PenFill cartridge delivery device (with or without the addition of a NovoPen® 3 PenMate®) with NovoFine® disposable needles
- 3 mL NovoLog FlexPen Prefilled Syringe
Contraindications
NovoLog is contraindicated
- during episodes of hypoglycemia
- in patients with hypersensitivity to NovoLog or one of its excipients.
Warnings and Precautions
Administration
NovoLog has a more rapid onset of action and a shorter duration of activity than regular human insulin. An injection of NovoLog should immediately be followed by a meal within 5-10 minutes. Because of NovoLog's short duration of action, a longer acting insulin should also be used in patients with type 1 diabetes and may also be needed in patients with type 2 diabetes. Glucose monitoring is recommended for all patients with diabetes and is particularly important for patients using external pump infusion therapy.
Any change of insulin dose should be made cautiously and only under medical supervision. Changing from one insulin product to another or changing the insulin strength may result in the need for a change in dosage. As with all insulin preparations, the time course of NovoLog action may vary in different individuals or at different times in the same individual and is dependent on many conditions, including the site of injection, local blood supply, temperature, and physical activity. Patients who change their level of physical activity or meal plan may require adjustment of insulin dosages. Insulin requirements may be altered during illness, emotional disturbances, or other stresses.
Patients using continuous subcutaneous insulin infusion pump therapy must be trained to administer insulin by injection and have alternate insulin therapy available in case of pump failure.
Hypoglycemia
Hypoglycemia is the most common adverse effect of all insulin therapies, including NovoLog. Severe hypoglycemia may lead to unconsciousness and/or convulsions and may result in temporary or permanent impairment of brain function or death. Severe hypoglycemia requiring the assistance of another person and/or parenteral glucose infusion or glucagon administration has been observed in clinical trials with insulin, including trials with NovoLog.
The timing of hypoglycemia usually reflects the time-action profile of the administered insulin formulations [see Clincal Pharmacology]. Other factors such as changes in food intake (e.g., amount of food or timing of meals), injection site, exercise, and concomitant medications may also alter the risk of hypoglycemia [see Drug Interactions]. As with all insulins, use caution in patients with hypoglycemia unawareness and in patients who may be predisposed to hypoglycemia (e.g., patients who are fasting or have erratic food intake). The patient's ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery.
Rapid changes in serum glucose levels may induce symptoms of hypoglycemia in persons with diabetes, regardless of the glucose value. Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as longstanding diabetes, diabetic nerve disease, use of medications such as beta-blockers, or intensified diabetes control [see Drug Interactions]. These situations may result in severe hypoglycemia (and, possibly, loss of consciousness) prior to the patient's awareness of hypoglycemia. Intravenously administered insulin has a more rapid onset of action than subcutaneously administered insulin, requiring more close monitoring for hypoglycemia.
Hypokalemia
All insulin products, including NovoLog, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia that, if left untreated, may cause respiratory paralysis, ventricular arrhythmia, and death. Use caution in patients who may be at risk for hypokalemia (e.g., patients using potassium-lowering medications, patients taking medications sensitive to serum potassium concentrations, and patients receiving intravenously administered insulin).
Renal Impairment
As with other insulins, the dose requirements for NovoLog may be reduced in patients with renal impairment [see Clinical Pharmacology].
Hepatic Impairment
As with other insulins, the dose requirements for NovoLog may be reduced in patients with hepatic impairment [see Clinical Pharmacology].
Hypersensitivity and Allergic Reactions
Local Reactions - As with other insulin therapy, patients may experience redness, swelling, or itching at the site of NovoLog injection. These reactions usually resolve in a few days to a few weeks, but in some occasions, may require discontinuation of NovoLog. In some instances, these reactions may be related to factors other than insulin, such as irritants in a skin cleansing agent or poor injection technique. Localized reactions and generalized myalgias have been reported with injected metacresol, which is an excipient in NovoLog.
Systemic Reactions - Severe, life-threatening, generalized allergy, including anaphylaxis, may occur with any insulin product, including NovoLog. Anaphylactic reactions with NovoLog have been reported post-approval. Generalized allergy to insulin may also cause whole body rash (including pruritus), dyspnea, wheezing, hypotension, tachycardia, or diaphoresis. In controlled clinical trials, allergic reactions were reported in 3 of 735 patients (0.4%) treated with regular human insulin and 10 of 1394 patients (0.7%) treated with NovoLog. In controlled and uncontrolled clinical trials, 3 of 2341 (0.1%) NovoLog-treated patients discontinued due to allergic reactions.
Antibody Production
Increases in anti-insulin antibody titers that react with both human insulin and insulin aspart have been observed in patients treated with NovoLog. Increases in anti-insulin antibodies are observed more frequently with NovoLog than with regular human insulin. Data from a 12-month controlled trial in patients with type 1 diabetes suggest that the increase in these antibodies is transient, and the differences in antibody levels between the regular human insulin and insulin aspart treatment groups observed at 3 and 6 months were no longer evident at 12 months. The clinical significance of these antibodies is not known. These antibodies do not appear to cause deterioration in glycemic control or necessitate increases in insulin dose.
Mixing of Insulins
- Mixing NovoLog with NPH human insulin immediately before injection attenuates the peak concentration of NovoLog, without significantly affecting the time to peak concentration or total bioavailability of NovoLog. If NovoLog is mixed with NPH human insulin, NovoLog should be drawn into the syringe first, and the mixture should be injected immediately after mixing.
- The efficacy and safety of mixing NovoLog with insulin preparations produced by other manufacturers have not been studied.
- Insulin mixtures should not be administered intravenously.
Continuous Subcutaneous Insulin Infusion by External Pump
When used in an external subcutaneous insulin infusion pump, NovoLog should not be mixed with any other insulin or diluent. When using NovoLog in an external insulin pump, the NovoLog-specific information should be followed (e.g., in-use time, frequency of changing infusion sets) because NovoLog-specific information may differ from general pump manual instructions.
Pump or infusion set malfunctions or insulin degradation can lead to a rapid onset of hyperglycemia and ketosis because of the small subcutaneous depot of insulin. This is especially pertinent for rapid-acting insulin analogs that are more rapidly absorbed through skin and have a shorter duration of action. Prompt identification and correction of the cause of hyperglycemia or ketosis is necessary. Interim therapy with subcutaneous injection may be required [see Dosage and Administration, Warnings and Precautions , and How Supplied/Storage and Handling].
NovoLog is recommended for use in pump systems suitable for insulin infusion as listed below.
Pumps:
MiniMed 500 series and other equivalent pumps.
Reservoirs and infusion sets:
NovoLog is recommended for use in reservoir and infusion sets that are compatible with insulin and the specific pump. In-vitro studies have shown that pump malfunction, loss of metacresol, and insulin degradation, may occur when NovoLog is maintained in a pump system for longer than 48 hours. Reservoirs and infusion sets should be changed at least every 48 hours.
NovoLog should not be exposed to temperatures greater than 37°C (98.6°F). NovoLog that will be used in a pump should not be mixed with other insulin or with a diluent [see Dosage and Administration, Warnings and Precautions, and How Supplied/Storage and Handling].
Adverse Reactions
Clinical Trial Experience
Because clinical trials are conducted under widely varying designs, the adverse reaction rates reported in one clinical trial may not be easily compared to those rates reported in another clinical trial, and may not reflect the rates actually observed in clinical practice.
- Hypoglycemia
Hypoglycemia is the most commonly observed adverse reaction in patients using insulin, including NovoLog [see Warnings and Precautions].
- Insulin initiation and glucose control intensification
Intensification or rapid improvement in glucose control has been associated with a transitory, reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acute painful peripheral neuropathy. However, long-term glycemic control decreases the risk of diabetic retinopathy and neuropathy.
- Lipodystrophy
Long-term use of insulin, including NovoLog, can cause lipodystrophy at the site of repeated insulin injections or infusion. Lipodystrophy includes lipohypertrophy (thickening of adipose tissue) and lipoatrophy (thinning of adipose tissue), and may affect insulin absorption. Rotate insulin injection or infusion sites within the same region to reduce the risk of lipodystrophy.
- Weight gain
Weight gain can occur with some insulin therapies, including NovoLog, and has been attributed to the anabolic effects of insulin and the decrease in glucosuria.
- Peripheral Edema
Insulin may cause sodium retention and edema, particularly if previously poor metabolic control is improved by intensified insulin therapy.
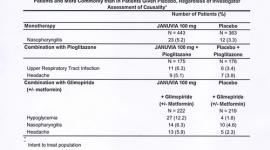
- Frequencies of adverse drug reactions
The frequencies of adverse drug reactions during NovoLog clinical trials in patients with type 1 diabetes mellitus and type 2 diabetes mellitus are listed in the tables below.
Table 1: Treatment-Emergent Adverse Events in Patients with Type 1 Diabetes Mellitus (Adverse events with frequency ≥ 5% and occurring more frequently with NovoLog compared to human regular insulin are listed)
| NovoLog + NPH N= 596 | Human Regular Insulin + NPH N= 286 | |||
| Preferred Term | N | (%) | N | (%) |
| Hypoglycemia * | 448 | 75% | 205 | 72% |
| Headache | 70 | 12% | 28 | 10% |
| Injury accidental | 65 | 11% | 29 | 10% |
| Nausea | 43 | 7% | 13 | 5% |
| Diarrhea | 28 | 5% | 9 | 3% |
* Hypoglycemia is defined as an episode of blood glucose concentration
Table 2: Treatment-Emergent Adverse Events in Patients with Type 2 Diabetes Mellitus (except for hypoglycemia, adverse events with frequency ≥ 5% and occurring more frequently with NovoLog compared to human regular insulin are listed)
| NovoLog + NPH N= 91 | Human Regular Insulin + NPH N= 91 | |||
| N | (%) | N | (%) | |
| Hypoglycemia* | 25 | 27% | 33 | 36% |
| Hyporeflexia | 10 | 11% | 6 | 7% |
| Onychomycosis | 9 | 10% | 5 | 5% |
| Sensory disturbance | 8 | 9% | 6 | 7% |
| Urinary tract infection | 7 | 8% | 6 | 7% |
| Chest pain | 5 | 5% | 3 | 3% |
| Headache | 5 | 5% | 3 | 3% |
| Skin disorder | 5 | 5% | 2 | 2% |
| Abdominal pain | 5 | 5% | 1 | 1% |
| Sinusitis | 5 | 5% | 1 | 1% |
* Hypoglycemia is defined as an episode of blood glucose concentration
Postmarketing Data
The following additional adverse reactions have been identified during postapproval use of NovoLog. Because these adverse reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency. Medication errors in which other insulins have been accidentally substituted for NovoLog have been identified during postapproval use.
Drug Interactions
A number of substances affect glucose metabolism and may require insulin dose adjustment and particularly close monitoring.
- The following are examples of substances that may increase the blood-glucose-lowering effect and susceptibility to hypoglycemia: oral antidiabetic products, pramlintide, ACE inhibitors, disopyramide, fibrates, fluoxetine, monoamine oxidase (MAO) inhibitors, propoxyphene, salicylates, somatostatin analog (e.g., octreotide), sulfonamide antibiotics.
- The following are examples of substances that may reduce the blood-glucose-lowering effect: corticosteroids, niacin, danazol, diuretics, sympathomimetic agents (e.g., epinephrine, salbutamol, terbutaline), isoniazid, phenothiazine derivatives, somatropin, thyroid hormones, estrogens, progestogens (e.g., in oral contraceptives), atypical antipsychotics.
- Beta-blockers, clonidine, lithium salts, and alcohol may either potentiate or weaken the blood-glucose-lowering effect of insulin.
- Pentamidine may cause hypoglycemia, which may sometimes be followed by hyperglycemia.
- The signs of hypoglycemia may be reduced or absent in patients taking sympatholytic products such as beta-blockers, clonidine, guanethidine, and reserpine.
Use in Specific Populations
Pregnancy
Pregnancy Category B. All pregnancies have a background risk of birth defects, loss, or other adverse outcome regardless of drug exposure. This background risk is increased in pregnancies complicated by hyperglycemia and may be decreased with good metabolic control. It is essential for patients with diabetes or history of gestational diabetes to maintain good metabolic control before conception and throughout pregnancy. Insulin requirements may decrease during the first trimester, generally increase during the second and third trimesters, and rapidly decline after delivery. Careful monitoring of glucose control is essential in these patients. Therefore, female patients should be advised to tell their physician if they intend to become, or if they become pregnant while taking NovoLog.
An open-label, randomized study compared the safety and efficacy of NovoLog (n=157) versus regular human insulin (n=165) in 322 pregnant women with type 1 diabetes. Two-thirds of the enrolled patients were already pregnant when they entered the study. Because only one-third of the patients enrolled before conception, the study was not large enough to evaluate the risk of congenital malformations. Both groups achieved a mean HbA1c of ~ 6% during pregnancy, and there was no significant difference in the incidence of maternal hypoglycemia.
Subcutaneous reproduction and teratology studies have been performed with NovoLog and regular human insulin in rats and rabbits. In these studies, NovoLog was given to female rats before mating, during mating, and throughout pregnancy, and to rabbits during organogenesis. The effects of NovoLog did not differ from those observed with subcutaneous regular human insulin. NovoLog, like human insulin, caused pre- and post-implantation losses and visceral/skeletal abnormalities in rats at a dose of 200 U/kg/day (approximately 32 times the human subcutaneous dose of 1.0 U/kg/day, based on U/body surface area) and in rabbits at a dose of 10 U/kg/day (approximately three times the human subcutaneous dose of 1.0 U/kg/day, based on U/body surface area). The effects are probably secondary to maternal hypoglycemia at high doses. No significant effects were observed in rats at a dose of 50 U/kg/day and in rabbits at a dose of 3 U/kg/day. These doses are approximately 8 times the human subcutaneous dose of 1.0 U/kg/day for rats and equal to the human subcutaneous dose of 1.0 U/kg/day for rabbits, based on U/body surface area.
Nursing Mothers
It is unknown whether insulin aspart is excreted in human milk. Use of NovoLog is compatible with breastfeeding, but women with diabetes who are lactating may require adjustments of their insulin doses.
Pediatric Use
NovoLog is approved for use in children for subcutaneous daily injections and for subcutaneous continuous infusion by external insulin pump. Please see Section CLINICAL STUDIES for summaries of clinical studies.
Geriatric Use
Of the total number of patients (n= 1,375) treated with NovoLog in 3 controlled clinical studies, 2.6% (n=36) were 65 years of age or over. One-half of these patients had type 1 diabetes (18/1285) and the other half had type 2 diabetes (18/90). The HbA1c response to NovoLog, as compared to human insulin, did not differ by age, particularly in patients with type 2 diabetes. Additional studies in larger populations of patients 65 years of age or over are needed to permit conclusions regarding the safety of NovoLog in elderly compared to younger patients. Pharmacokinetic/pharmacodynamic studies to assess the effect of age on the onset of NovoLog action have not been performed.
Overdosage
Excess insulin administration may cause hypoglycemia and, particularly when given intravenously, hypokalemia. Mild episodes of hypoglycemia usually can be treated with oral glucose. Adjustments in drug dosage, meal patterns, or exercise, may be needed. More severe episodes with coma, seizure, or neurologic impairment may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. Sustained carbohydrate intake and observation may be necessary because hypoglycemia may recur after apparent clinical recovery. Hypokalemia must be corrected appropriately.
Description
NovoLog (insulin aspart [rDNA origin] injection) is a rapid-acting human insulin analog used to lower blood glucose. NovoLog is homologous with regular human insulin with the exception of a single substitution of the amino acid proline by aspartic acid in position B28, and is produced by recombinant DNA technology utilizing Saccharomyces cerevisiae (baker's yeast). Insulin aspart has the empirical formula C256H381N65079S6 and a molecular weight of 5825.8.

Figure 1. Structural formula of insulin aspart.
NovoLog is a sterile, aqueous, clear, and colorless solution, that contains insulin aspart 100 Units/mL, glycerin 16 mg/mL, phenol 1.50 mg/mL, metacresol 1.72 mg/mL, zinc 19.6 mcg/mL, disodium hydrogen phosphate dihydrate 1.25 mg/mL, and sodium chloride 0.58 mg/mL. NovoLog has a pH of 7.2-7.6. Hydrochloric acid 10% and/or sodium hydroxide 10% may be added to adjust pH.
Clinical Pharmacology
Mechanism Of Action
The primary activity of NovoLog is the regulation of glucose metabolism. Insulins, including NovoLog, bind to the insulin receptors on muscle and fat cells and lower blood glucose by facilitating the cellular uptake of glucose and simultaneously inhibiting the output of glucose from the liver.
Pharmacodynamics
Studies in normal volunteers and patients with diabetes demonstrated that subcutaneous administration of NovoLog has a more rapid onset of action than regular human insulin.
In a study in patients with type 1 diabetes (n=22), the maximum glucose-lowering effect of NovoLog occurred between 1 and 3 hours after subcutaneous injection (see Figure 2). The duration of action for NovoLog is 3 to 5 hours. The time course of action of insulin and insulin analogs such as NovoLog may vary considerably in different individuals or within the same individual. The parameters of NovoLog activity (time of onset, peak time and duration) as designated in Figure 2 should be considered only as general guidelines. The rate of insulin absorption and onset of activity is affected by the site of injection, exercise, and other variables [see Warnings and Precautions].

Figure 2. Serial mean serum glucose collected up to 6 hours following a single pre-meal dose of NovoLog (solid curve) or regular human insulin (hatched curve) injected immediately before a meal in 22 patients with type 1 diabetes.
A double-blind, randomized, two-way cross-over study in 16 patients with type 1 diabetes demonstrated that intravenous infusion of NovoLog resulted in a blood glucose profile that was similar to that after intravenous infusion with regular human insulin. NovoLog or human insulin was infused until the patient's blood glucose decreased to 36 mg/dL, or until the patient demonstrated signs of hypoglycemia (rise in heart rate and onset of sweating), defined as the time of autonomic reaction (R) (see Figure 3).

Figure 3. Serial mean serum glucose following intravenous infusion of NovoLog (hatched curve) and regular human insulin (solid curve) in 16 patients with type 1 diabetes. R represents the time of autonomic reaction.
Pharmacokinetics
The single substitution of the amino acid proline with aspartic acid at position B28 in NovoLog reduces the molecule's tendency to form hexamers as observed with regular human insulin. NovoLog is, therefore, more rapidly absorbed after subcutaneous injection compared to regular human insulin.
In a randomized, double-blind, crossover study 17 healthy Caucasian male subjects between 18 and 40 years of age received an intravenous infusion of either NovoLog or regular human insulin at 1.5 mU/kg/min for 120 minutes. The mean insulin clearance was similar for the two groups with mean values of 1.2 l/h/kg for the NovoLog group and 1.2 l/h/kg for the regular human insulin group.
Bioavailability and Absorption - NovoLog has a faster absorption, a faster onset of action, and a shorter duration of action than regular human insulin after subcutaneous injection (see Figure 2 and Figure 4). The relative bioavailability of NovoLog compared to regular human insulin indicates that the two insulins are absorbed to a similar extent.

Figure 4. Serial mean serum free insulin concentration collected up to 6 hours following a single pre-meal dose of NovoLog (solid curve) or regular human insulin (hatched curve) injected immediately before a meal in 22 patients with type 1 diabetes.
In studies in healthy volunteers (total n=l07) and patients with type 1 diabetes (total n=40), NovoLog consistently reached peak serum concentrations approximately twice as fast as regular human insulin. The median time to maximum concentration in these trials was 40 to 50 minutes for NovoLog versus 80 to 120 minutes for regular human insulin. In a clinical trial in patients with type 1 diabetes, NovoLog and regular human insulin, both administered subcutaneously at a dose of 0.15 U/kg body weight, reached mean maximum concentrations of 82 and 36 mU/L, respectively. Pharmacokinetic/pharmacodynamic characteristics of insulin aspart have not been established in patients with type 2 diabetes.
The intra-individual variability in time to maximum serum insulin concentration for healthy male volunteers was significantly less for NovoLog than for regular human insulin. The clinical significance of this observation has not been established.
In a clinical study in healthy non-obese subjects, the pharmacokinetic differences between NovoLog and regular human insulin described above, were observed independent of the site of injection (abdomen, thigh, or upper arm).
Distribution and Elimination - NovoLog has low binding to plasma proteins (<10%), similar to that seen with regular human insulin. After subcutaneous administration in normal male volunteers (n=24), NovoLog was more rapidly eliminated than regular human insulin with an average apparent half-life of 81 minutes compared to 141 minutes for regular human insulin.
Specific Populations
Children and Adolescents - The pharmacokinetic and pharmacodynamic properties of NovoLog and regular human insulin were evaluated in a single dose study in 18 children (6-12 years, n=9) and adolescents (13-17 years [Tanner grade > 2], n=9) with type 1 diabetes. The relative differences in pharmacokinetics and pharmacodynamics in children and adolescents with type 1 diabetes between NovoLog and regular human insulin were similar to those in healthy adult subjects and adults with type 1 diabetes.
Gender - In healthy volunteers, no difference in insulin aspart levels was seen between men and women when body weight differences were taken into account. There was no significant difference in efficacy noted (as assessed by HbAlc) between genders in a trial in patients with type 1 diabetes.
Obesity - A single subcutaneous dose of 0.1 U/kg NovoLog was administered in a study of 23 patients with type 1 diabetes and a wide range of body mass index (BMI, 22-39 kg/m2). The pharmacokinetic parameters, AUC and Cmax, of NovoLog were generally unaffected by BMI in the different groups - BMI 19-23 kg/m2 (N=4); BMI 23-27 kg/m2 (N=7); BMI 27-32 kg/m2 (N=6) and BMI >32 kg/m2 (N=6). Clearance of NovoLog was reduced by 28% in patients with BMI >32 kg/m2 compared to patients with BMI
Renal Impairment - Some studies with human insulin have shown increased circulating levels of insulin in patients with renal failure. A single subcutaneous dose of 0.08 U/kg NovoLog was administered in a study to subjects with either normal (N=6) creatinine clearance (CLcr) (> 80 ml/min) or mild (N=7; CLcr = 50-80 ml/min), moderate (N=3; CLcr = 30-50 ml/min) or severe (but not requiring hemodialysis) (N=2; CLcr = Warnings and Precautions].
Hepatic Impairment - Some studies with human insulin have shown increased circulating levels of insulin in patients with liver failure. A single subcutaneous dose of 0.06 U/kg NovoLog was administered in an open-label, single-dose study of 24 subjects (N=6/group) with different degree of hepatic impairment (mild, moderate and severe) having Child-Pugh Scores ranging from 0 (healthy volunteers) to 12 (severe hepatic impairment). In this small study, there was no correlation between the degree of hepatic failure and any NovoLog pharmacokinetic parameter. Careful glucose monitoring and dose adjustments of insulin, including NovoLog, may be necessary in patients with hepatic dysfunction [see Warnings and Precautions].
The effect of age, ethnic origin, pregnancy and smoking on the pharmacokinetics and pharmacodynamics of NovoLog has not been studied.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment Of Fertility
Standard 2-year carcinogenicity studies in animals have not been performed to evaluate the carcinogenic potential of NovoLog. In 52-week studies, Sprague-Dawley rats were dosed subcutaneously with NovoLog at 10, 50, and 200 U/kg/day (approximately 2, 8, and 32 times the human subcutaneous dose of 1.0 U/kg/day, based on U/body surface area, respectively). At a dose of 200 U/kg/day, NovoLog increased the incidence of mammary gland tumors in females when compared to untreated controls. The incidence of mammary tumors for NovoLog was not significantly different than for regular human insulin. The relevance of these findings to humans is not known. NovoLog was not genotoxic in the following tests: Ames test, mouse lymphoma cell forward gene mutation test, human peripheral blood lymphocyte chromosome aberration test, in vivo micronucleus test in mice, and in ex vivo UDS test in rat liver hepatocytes. In fertility studies in male and female rats, at subcutaneous doses up to 200 U/kg/day (approximately 32 times the human subcutaneous dose, based on U/body surface area), no direct adverse effects on male and female fertility, or general reproductive performance of animals was observed.
Animal Toxicology And/Or Pharmacology
In standard biological assays in mice and rabbits, one unit of NovoLog has the same glucose-lowering effect as one unit of regular human insulin. In humans, the effect of NovoLog is more rapid in onset and of shorter duration, compared to regular human insulin, due to its faster absorption after subcutaneous injection (see Section CLINICAL PHARMACOLOGY Figure 2 and Figure 4).
Clinical Studies
Subcutaneous Daily Injections
Two six-month, open-label, active-controlled studies were conducted to compare the safety and efficacy of NovoLog to Novolin R in adult patients with type 1 diabetes. Because the two study designs and results were similar, data are shown for only one study (see Table 3). NovoLog was administered by subcutaneous injection immediately prior to meals and regular human insulin was administered by subcutaneous injection 30 minutes before meals. NPH insulin was administered as the basal insulin in either single or divided daily doses. Changes in HbA1c and the incidence rates of severe hypoglycemia (as determined from the number of events requiring intervention from a third party) were comparable for the two treatment regimens in this study (Table 3) as well as in the other clinical studies that are cited in this section. Diabetic ketoacidosis was not reported in any of the adult studies in either treatment group.
Table 3. Subcutaneous NovoLog Administration in Type 1 Diabetes (24 weeks; n=882)
| NovoLog + NPH | Novolin R + NPH | |
| N | 596 | 286 |
| Baseline HbA1c (%)* | 7.9 ±1.1 | 8.0 ± 1.2 |
| Change from Baseline HbA1c (%) | -0.1 ± 0.8 | 0.0 ± 0.8 |
| Treatment Difference in HbA1c ,Mean (95% confidence interval) | -0.2 (-0.3, -0.1) | |
| Baseline insulin dose (IU/kg/24 hours)* | 0.7 ± 0.2 | 0.7 ± 0.2 |
| End-of-Study insulin dose (IU/kg/24 hours)* | 0.7 ± 0.2 | 0.7 ± 0.2 |
| Patients with severe hypoglycemia (n, %)†| 104 (17%) | 54 (19%) |
| Baseline body weight (kg)* Weight Change from baseline (kg)* | 75.3 ± 14.5 0.5 ± 3.3 | 75.9 ± 13.1 0.9 ± 2.9 |
* Values are Mean ± SD
†Severe hypoglycemia refers to hypoglycemia associated with central nervous system symptoms and requiring the intervention of another person or hospitalization.
A 24-week, parallel-group study of children and adolescents with type 1 diabetes (n = 283) aged 6 to 18 years compared two subcutaneous multiple-dose treatment regimens: NovoLog (n = 187) or Novolin R (n = 96). NPH insulin was administered as the basal insulin. NovoLog achieved glycemic control comparable to Novolin R, as measured by change in HbA1c (Table 4) and both treatment groups had a comparable incidence of hypoglycemia. Subcutaneous administration of NovoLog and regular human insulin have also been compared in children with type 1 diabetes (n=26) aged 2 to 6 years with similar effects on HbA1c and hypoglycemia.
Table 4. Pediatric Subcutaneous Administration of NovoLog in Type 1 Diabetes (24 weeks; n=283)
| NovoLog + NPH | Novolin R + NPH | |
| N | 187 | 96 |
| Baseline HbA1c (%) * | 8.3 ± 1.2 | 8.3 ± 1.3 |
| Change from Baseline HbA1c (%) | 0.1 ± 1.0 | 0.1 ± 1.1 |
| Treatment Difference in HbA1c, Mean (95% confidence interval) | 0.1 (-0.5, 0.1) | |
| Baseline insulin dose (IU/kg/24 hours) * | 0.4 ± 0.2 | 0.6 ± 0.2 |
| End-of-Study insulin dose (IU/kg/24 hours) * | 0.4 ± 0.2 | 0.7 ± 0.2 |
| Patients with severe hypoglycemia (n, %)†| 11 (6%) | 9 (9%) |
| Diabetic ketoacidosis (n, %) | 10 (5%) | 2 (2%) |
| Baseline body weight (kg) * Weight Change from baseline (kg) * | 50.6 ± 19.6 2.7 ± 3.5 | 48.7 ± 15.8 2.4 ± 2.6 |
* Values are Mean ± SD
†Severe hypoglycemia refers to hypoglycemia associated with central nervous system symptoms and requiring the intervention of another person or hospitalization.
One six-month, open-label, active-controlled study was conducted to compare the safety and efficacy of NovoLog to Novolin R in patients with type 2 diabetes (Table 5). NovoLog was administered by subcutaneous injection immediately prior to meals and regular human insulin was administered by subcutaneous injection 30 minutes before meals. NPH insulin was administered as the basal insulin in either single or divided daily doses. Changes in HbAlc and the rates of severe hypoglycemia (as determined from the number of events requiring intervention from a third party) were comparable for the two treatment regimens.
Table 5. Subcutaneous NovoLog Administration in Type 2 Diabetes (6 months; n=176)
| NovoLog + NPH | Novolin R + NPH | |
| N | 90 | 86 |
| Baseline HbA1c (%) * | 8.1 ± 1.2 | 7.8 ± 1.1 |
| Change from Baseline HbA1c (%) | -0.3 ± 1.0 | -0.1 ± 0.8 |
| Treatment Difference in HbA1c, Mean (95% confidence interval) | - 0.1 (-0.4, -0.1) | |
| Baseline insulin dose (IU/kg/24 hours) * | 0.6 ± 0.3 | 0.6 ± 0.3 |
| End-of-Study insulin dose (IU/kg/24 hours) * | 0.7 ± 0.3 | 0.7 ± 0.3 |
| Patients with severe hypoglycemia (n, %) †| 9 (10%) | 5 (8%) |
| Baseline body weight (kg) * Weight Change from baseline (kg) * | 88.4 ± 13.3 1.2 ± 3.0 | 85.8 ± 14.8 0.4 ± 3.1 |
* Values are Mean ± SD
†Severe hypoglycemia refers to hypoglycemia associated with central nervous system symptoms and requiring the intervention of another person or hospitalization.
Continuous Subcutaneous Insulin Infusion (CSII) by External Pump
Two open-label, parallel design studies (6 weeks [n=29] and 16 weeks [n=118]) compared NovoLog to buffered regular human insulin (Velosulin) in adults with type 1 diabetes receiving a subcutaneous infusion with an external insulin pump. The two treatment regimens had comparable changes in HbA1c and rates of severe hypoglycemia.
Table 6. Adult Insulin Pump Study in Type 1 Diabetes (16 weeks; n=118)
| NovoLog | Buffered human insulin | |
| N | 59 | 59 |
| Baseline HbA1c (%) * | 7.3 ± 0.7 | 7.5 ± 0.8 |
| Change from Baseline HbA1c (%) | 0.0 ± 0.5 | 0.2 ± 0.6 |
| Treatment Difference in HbA1c, Mean (95% confidence interval) | 0.3 (-0.1, 0.4) | |
| Baseline insulin dose (IU/kg/24 hours) * | 0.7 ± 0.8 | 0.6 ± 0.2 |
| End-of-Study insulin dose (IU/kg/24 hours) * | 0.7 ± 0.7 | 0.6 ± 0.2 |
| Patients with severe hypoglycemia (n, %) †| 1 (2%) | 2 (3%) |
| Baseline body weight (kg) * Weight Change from baseline (kg) * | 77.4 ± 16.1 0.1 ± 3.5 | 74.8 ± 13.8 -0.0 ± 1.7 |
* Values are Mean ± SD
†Severe hypoglycemia refers to hypoglycemia associated with central nervous system symptoms and requiring the intervention of another person or hospitalization.
A randomized, 16-week, open-label, parallel design study of children and adolescents with type 1 diabetes (n=298) aged 4-18 years compared two subcutaneous infusion regimens administered via an external insulin pump: NovoLog (n=198) or insulin lispro (n=100). These two treatments resulted in comparable changes from baseline in HbA1c and comparable rates of hypoglycemia after 16 weeks of treatment (see Table 7).
Table 7. Pediatric Insulin Pump Study in Type 1 Diabetes (16 weeks; n=298)
| NovoLog | Lispro | |
| N | 198 | 100 |
| Baseline HbA1c (%) * | 8.0 ± 0.9 | 8.2 ± 0.8 |
| Change from Baseline HbA1c (%) | -0.1 ± 0.8 | -0.1 ± 0.7 |
| Treatment Difference in HbA1c, Mean (95% confidence interval) | -0.1 (-0.3, 0.1) | |
| Baseline insulin dose (IU/kg/24 hours) * | 0.9 ± 0.3 | 0.9 ± 0.3 |
| End-of-Study insulin dose (IU/kg/24 hours) * | 0.9 ± 0.2 | 0.9 ± 0.2 |
| Patients with severe hypoglycemia (n, %) †| 19 (10%) | 8 (8%) |
| Diabetic ketoacidosis (n, %) | 1 (0.5%) | 0 (0) |
| Baseline body weight (kg) * Weight Change from baseline (kg) * | 54.1 ± 19.7 1.8 ± 2.1 | 55.5 ± 19.0 1.6 ± 2.1 |
* Values are Mean ± SD
†Severe hypoglycemia refers to hypoglycemia associated with central nervous system symptoms and requiring the intervention of another person or hospitalization.
An open-label, 16-week parallel design trial compared pre-prandial NovoLog injection in conjunction with NPH injections to NovoLog administered by continuous subcutaneous infusion in 127 adults with type 2 diabetes. The two treatment groups had similar reductions in HbA1c and rates of severe hypoglycemia (Table 8) [see Indications and Usage, Dosage and Administration, Warnings and Precautions and How Supplied/Storage and Handling].
Table 8. Pump Therapy in Type 2 Diabetes (16 weeks; n=127)
| NovoLog pump | NovoLog + NPH | |
| N | 66 | 61 |
| Baseline HbA1c (%) * | 8.2 ± 1.4 | 8.0 ± 1.1 |
| Change from Baseline HbA1c (%) | -0.6 ± 1.1 | -0.5 ± 0.9 |
| Treatment Difference in HbA1c, Mean (95% confidence interval) | 0.1 (0.4, 0.3) | |
| Baseline insulin dose (IU/kg/24 hours) * | 0.7 ± 0.3 | 0.8 ± 0.5 |
| End-of-Study insulin dose (IU/kg/24 hours) * | 0.9 ± 0.4 | 0.9 ± 0.5 |
| Baseline body weight (kg) * Weight Change from baseline (kg) * | 96.4 ± 17.0 1.7 ± 3.7 | 96.9 ± 17.9 0.7 ± 4.1 |
* Values are Mean ± SD
Intravenous Administration of NovoLog
See Section Clinical Pharmacology/Pharmacodynamics.
How Supplied /Storage and Handling
NovoLog is available in the following package sizes: each presentation containing 100 Units of insulin aspart per mL (U-100).
| 10 mL vials | NDC 0169-7501-11 |
| 3 mL PenFill cartridges* | NDC 0169-3303-12 |
| 3 mL NovoLog FlexPen Prefilled syringe | NDC 0169-6339-10 |
* NovoLog PenFill cartridges are designed for use with Novo Nordisk 3 mL PenFill cartridge compatible insulin delivery devices (with or without the addition of a NovoPen 3 PenMate) with NovoFine disposable needles.
Recommended Storage
Unused NovoLog should be stored in a refrigerator between 2° and 8°C (36° to 46°F). Do not store in the freezer or directly adjacent to the refrigerator cooling element. Do not freeze NovoLog and do not use NovoLog if it has been frozen. NovoLog should not be drawn into a syringe and stored for later use.
Vials: After initial use a vial may be kept at temperatures below 30°C (86°F) for up to 28 days, but should not be exposed to excessive heat or sunlight. Opened vials may be refrigerated.
Unpunctured vials can be used until the expiration date printed on the label if they are stored in a refrigerator. Keep unused vials in the carton so they will stay clean and protected from light.
PenFill cartridges or NovoLog FlexPen Prefilled Syringes:
Once a cartridge or a NovoLog FlexPen Prefilled syringe is punctured, it should be kept at temperatures below 30°C (86°F) for up to 28 days, but should not be exposed to excessive heat or sunlight. Cartridges or NovoLog FlexPen Prefilled syringes in use must NOT be stored in the refrigerator. Keep all PenFill® cartridges and disposable NovoLog FlexPen Prefilled syringes away from direct heat and sunlight. Unpunctured PenFill cartridges and NovoLog FlexPen Prefilled syringes can be used until the expiration date printed on the label if they are stored in a refrigerator. Keep unused PenFill cartridges and NovoLog FlexPen Prefilled syringes in the carton so they will stay clean and protected from light.
Always remove the needle after each injection and store the 3 mL PenFill cartridge delivery device or NovoLog FlexPen Prefilled Syringe without a needle attached. This prevents contamination and/or infection, or leakage of insulin, and will ensure accurate dosing. Always use a new needle for each injection to prevent contamination.
Pump:
NovoLog in the pump reservoir should be discarded after at least every 48 hours of use or after exposure to temperatures that exceed 37°C (98.6°F).
Summary of Storage Conditions:
The storage conditions are summarized in the following table:
Table 9. Storage conditions for vial, PenFill cartridges and NovoLog FlexPen Prefilled syringe
| NovoLog presentation | Not in-use (unopened) Room Temperature (below 30°C) | Not in-use (unopened) Refrigerated | In-use (opened) Room Temperature (below 30°C) |
| 10 mL vial | 28 days | Until expiration date | 28 days (refrigerated/room temperature) |
| 3 mL PenFill cartridges | 28 days | Until expiration date | 28 days (Do not refrigerate) |
| 3 mL NovoLog FlexPen Prefilled syringe | 28 days | Until expiration date | 28 days (Do not refrigerate) |
Storage of Diluted NovoLog
NovoLog diluted with Insulin Diluting Medium for NovoLog to a concentration equivalent to U-10 or equivalent to U-50 may remain in patient use at temperatures below 30°C (86°F) for 28 days.
Storage of NovoLog in Infusion Fluids
Infusion bags prepared as indicated under Dosage and Administration (2) are stable at room temperature for 24 hours. Some insulin will be initially adsorbed to the material of the infusion bag.
last updated 12/2008
NovoLog, insulin aspart, patient information (in plain English)
Detailed Info on Signs, Symptoms, Causes, Treatments of Diabetes
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse.
back to: Browse all Medications for Diabetes
APA Reference
Staff, H.
(2008, December 31). NovoLog for Treatment of Diabetes - Novolog Full Prescribing Information, HealthyPlace. Retrieved
on 2025, April 15 from https://www.healthyplace.com/diabetes/medications/novolog-insulin-pump-information