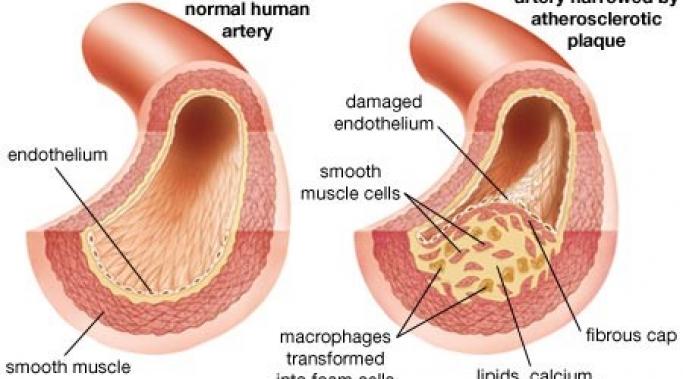
New research indicates that older veterans with combat posttraumatic stress disorder (PTSD) are at greater risk for vascular disease. We know that combat PTSD affects the brain and the body in a myriad of ways and now we are coming to understand that one of these ways is vascular.
Understanding Combat PTSD
For veterans, unemployment is the biggest predictor of posttraumatic stress disorder (PTSD) symptom severity, says a new study. The PTSD symptoms may be combat-PTSD-related or sexual-trauma-related, but either way, veteran unemployment predicts the severity of PTSD symptoms more than even indicators like depression. Organizations that employ veterans, like the one I mention below, may actually help those suffering from combat PTSD.
Military sexual trauma is a risk factor for posttraumatic stress disorder (PTSD) and other mental illnesses; and, unfortunately, sexual trauma is unusually common in the military. The Veteran’s Administration has implemented universal initiatives for the screening of military sexual trauma, but is this enough to help veterans who experience sexual trauma and PTSD?
There is a prevalent, and false, assumption that all veterans have posttraumatic stress disorder (PTSD), or, perhaps, all veterans who have experienced combat suffer from combat PTSD. This, though, is not the case. A recent study of United States veterans now shows quite clearly that while the rate of PTSD in veterans is high, the PTSD rate in veterans is not nearly as high in all populations.
While it’s something that many people don’t want to talk about, sex matters to people. Sexual function and sexual desire can be important parts of a person’s life, particularly if he or she is in a relationship. And, unfortunately, what we know is that combat posttraumatic stress disorder (PTSD) affects a veteran’s sexual desire and sexual function in negative ways. In fact, some studies have showed such a correlation between sexual dysfunction and PTSD that some have proposed making it an official, diagnostic criteria.
There is stigma in our society around combat veterans with PTSD (combat posttraumatic stress disorder [PTSD]). Stigma consists of negative stereotypes of people simply because of a diagnosis and these unfair perceptions affect not only a veteran’s relationship with others but also the veteran’s relationship to his or herself.
There is no shortage of triggers for veterans with combat posttraumatic stress disorder (PTSD) during the holidays. Loud noises, parties with crowds of people, the expectations of positive emotions and so many more things can make combat PTSD harder to live with during the holidays; and when everyone around you is having a great time, it can feel very lonely being the one who feels worse during the holiday celebrations. But there is hope. Use these tips to handle your PTSD during the holidays and maybe even have some fun.
On Understanding Combat PTSD I focus on the issues surrounding combat posttraumatic stress disorder (PTSD), often from a medical perspective. However, there are many people that have views on combat PTSD outside of doctors. Of course, veterans are one of these groups and some veterans (and others) might argue that PTSD is not, in fact, a disorder. Why would people think that?
A few weeks ago, I discussed how hyperarousal (or feeling “keyed up”) is a symptom area of combat posttraumatic stress disorder (PTSD). A symptom that is part of hyperarousal is an exaggerated startle response. But what is this response and what might this PTSD symptom look like?
This blog is specifically geared toward combat-related posttraumatic stress disorder (PTSD), however, there are many people outside of this situation who also suffer from PTSD. This blog is not meant to suggest that this significant group of people doesn’t exist. Here is some information about PTSD in multiple populations.