J. Jaffe (Ed.), Encyclopedia of Drugs and Alcohol, New York: Macmillan, pp. 92-97 (written in 1991, references updated 1993)

Abstinence is the total avoidance of an activity. It is the dominant approach in the United States to resolving alcoholism and drug abuse (e.g., "Just Say No"). Abstinence was at the base of Prohibition (legalized in 1919 with the Eighteenth Amendment) and is closely related to prohibitionism—the legal proscription of substances and their use.
Although temperance originally meant moderation, the nineteenth-century TEMPERANCE MOVEMENT'S emphasis on complete abstinence from alcohol and the mid-twentieth century's experience of the ALCOHOLICS ANONYMOUS movement have strongly influenced alcohol- and drug-abuse treatment goals in the United States. Moral and clinical issues have been irrevocably mixed.
The disease model of alcoholism and drug addiction, which insists on abstinence, has incorporated new areas of compulsive behavior—such as overeating and sexual involvements. In these cases, redefinition of abstinence to mean "the avoidance of excess" (what we would otherwise term moderation) is required.
Abstinence can also be used as a treatment-outcome measure, as an indicator of its effectiveness. In this case, abstinence is defined as the number of drug-free days or weeks during the treatment regimen—and measures of drug in urine are often used as objective indicators.
Bibliography
HEATH, D.B. (1992). Prohibition or liberalization of alcohol and drugs? In M. Galanter (Ed.), Recent developments in alcoholism Alcohol and cocaine. New York: Plenum.
LENDER, M. E., & MARTIN, J. K. (1982). Drinking in America. New York: Free Press.
PEELE, S., BRODSKY, A., & ARNOLD, M. (1991). The truth about addiction and recovery. New York: Simon & Schuster.
Controlled Drinking versus Abstinence
Stanton Peele
The position of ALCOHOLICS ANONYMOUS (AA) and the dominant view among therapists who treat alcoholism in the United States is that the goal of treatment for those who have been dependent on alcohol is total, complete, and permanent abstinence from alcohol (and, often, other intoxicating substances). By extension, for all those treated for alcohol abuse, including those with no dependence symptoms, moderation of drinking (termed controlled drinking or CD) as a goal of treatment is rejected (Peele, 1992). Instead, providers claim, holding out such a goal to an alcoholic is detrimental, fostering a continuation of denial and delaying the alcoholic's need to accept the reality that he or she can never drink in moderation.
In Britain and other European and Commonwealth countries, controlled-drinking therapy is widely available (Rosenberg et al., 1992). The following six questions explore the value, prevalence, and clinical impact of controlled drinking versus abstinence outcomes in alcoholism treatment; they are intended to argue the case for controlled drinking as a reasonable and realistic goal.
1. What proportion of treated alcoholics abstain completely following treatment?
At one extreme, Vaillant (1983) found a 95 percent relapse rate among a group of alcoholics followed for 8 years after treatment at a public hospital; and over a 4-year follow-up period, the Rand Corporation found that only 7 percent of a treated alcoholic population abstained completely (Polich, Armor, & Braiker, 1981). At the other extreme, Wallace et al. (1988) reported a 57 percent continuous abstinence rate for private clinic patients who were stably married and had successfully completed detoxification and treatment—but results in this study covered only a 6-month period.
In other studies of private treatment, Walsh et al. (1991) found that only 23 percent of alcohol-abusing workers reported abstaining throughout a 2-year follow-up, although the figure was 37 percent for those assigned to a hospital program. According to Finney and Moos (1991), 37 percent of patients reported they were abstinent at all follow-up years 4 through 10 after treatment. Clearly, most research agrees that most alcoholism patients drink at some point following treatment.
2. What proportion of alcoholics eventually achieve abstinence following alcoholism treatment?
Many patients ultimately achieve abstinence only over time. Finney and Moos (1991) found that 49 percent of patients reported they were abstinent at 4 years and 54 percent at 10 years after treatment. Vaillant (1983) found that 39 percent of his surviving patients were abstaining at 8 years. In the Rand study, 28 percent of assessed patients were abstaining after 4 years. Helzer et al. (1985), however, reported that only 15 percent of all surviving alcoholics seen in hospitals were abstinent at 5 to 7 years. (Only a portion of these patients were specifically treated in an alcoholism unit. Abstinence rates were not reported separately for this group, but only 7 percent survived and were in remission at follow-up.)
3. What is the relationship of abstinence to controlled-drinking outcomes over time?
Edwards et al. (1983) reported that controlled drinking is more unstable than abstinence for alcoholics over time, but recent studies have found that controlled drinking increases over longer follow-up periods. Finney and Moos (1991) reported a 17 percent "social or moderate drinking" rate at 6 years and a 24 percent rate at 10 years. In studies by McCabe (1986) and Nordström and Berglund (1987), CD outcomes exceeded abstinence during follow-up of patients 15 and more years after treatment (see Table 1). Hyman (1976) earlier found a similar emergence of controlled drinking over 15 years.
4. What are legitimate nonabstinent outcomes for alcoholism?
The range of nonabstinence outcomes between unabated alcoholism and total abstinence includes (I) "improved drinking" despite continuing alcohol abuse, (2) "largely controlled drinking" with occasional relapses, and (3) "completely controlled drinking." Yet some studies count both groups (1) and (2) as continuing alcoholics and those in group (3) who engage in only occasional drinking as abstinent. Vaillant (1983) labeled abstinence as drinking less than once a month and including a binge lasting less than a week each year.
The importance of definitional criteria is evident in a highly publicized study (Helzer et al., 1985) that identified only 1.6 percent Of treated alcoholism patients as "moderate drinkers." Not included in this category were an additional 4.6 percent of patients who drank without problems but who drank in fewer than 30 of the previous 36 months. In addition, Helzer et al. identified a sizable group (12%) of former alcoholics who drank a threshold of 7 drinks 4 times in a single month over the previous 3 years but who reported no adverse consequences or symptoms of alcohol dependence and for whom no such problems were uncovered from collateral records. Nonetheless, Helzer et al. rejected the value of CD outcomes in alcoholism treatment.
While the Helzer et al. study was welcomed by the American treatment industry, the Rand results (Polich, Armor, & Braiker, 1981) were publicly denounced by alcoholism treatment advocates. Yet the studies differed primarily in that Rand reported a higher abstinence rate, using a 6-month window at assessment (compared with 3 years for Helzer et al.). The studies found remarkably similar nonabstinence outcomes, but Polich, Armor, and Braiker (1981) classified both occasional and continuous moderate drinkers (8%) and sometimes heavy drinkers (10%) who had no negative drinking consequences or dependence symptoms in a nonabstinent remission category. (Rand subjects had been highly alcoholic and at intake were consuming a median of 17 drinks daily.)
The harm-reduction approach seeks to minimize the damage from continued drinking and recognizes a wide range of improved categories (Heather, 1992). Minimizing nonabstinent remission or improvement categories by labeling reduced but occasionally excessive drinking as "alcoholism" fails to address the morbidity associated with continued untrammeled drinking.
5. How do untreated and treated alcoholics compare in their controlled-drinking and abstinent-remission ratios?
Alcoholic remission many years after treatment may depend less on treatment than on posttreatment experiences, and in some long-term studies, CD outcomes become more prominent the longer subjects are out of the treatment milieu, because patients unlearn the abstinence prescription that prevails there (Peele, 1987). By the same token, controlled drinking may be the more common outcome for untreated remission, since many alcohol abusers may reject treatment because they are unwilling to abstain.
Goodwin, Crane, & Guze (1971) found that controlled-drinking remission was four times as frequent as abstinence after eight years for untreated alcoholic felons who had "unequivocal histories of alcoholism" (see Table 1). Results from the 1989 Canadian National Alcohol and Drug Survey confirmed that those who resolve a drinking problem without treatment are more likely to become controlled drinkers. Only 18 percent of 500 recovered alcohol abusers in the survey achieved remission through treatment. About half (49%) of those in remission still drank. Of those in remission through treatment, 92 percent were abstinent. But 61 percent of those who achieved remission without treatment continued drinking (see Table 2).
6. For which alcohol abusers is controlled-drinking therapy or abstinence therapy superior?
Severity of alcoholism is the most generally accepted clinical indicator of the appropriateness of CD therapy (Rosenberg, 1993). Untreated alcohol abusers probably have less severe drinking problems than clinical populations of alcoholics, which may explain their higher levels of controlled drinking. But the less severe problem drinkers uncovered in nonclinical studies are more typical, outnumbering those who "show major symptoms of alcohol dependence" by about four to one (Skinner, 1990).
Despite the reported relationship between severity and CD outcomes, many diagnosed alcoholics do control their drinking, as Table 1 reveals. The Rand study quantified the relationship between severity of alcohol dependence and controlled-drinking outcomes, although, overall, the Rand population was a severely alcoholic one in which "virtually all subjects reported symptoms of alcohol dependence" (Polich, Armor, and Braiker, 1981).
Polich, Armor, and Braiker found that the most severely dependent alcoholics (11 or more dependence symptoms on admission) were the least likely to achieve nonproblem drinking at 4 years. However, a quarter or this group who achieved remission did so through nonproblem drinking. Furthermore, younger (under 40), single alcoholics were far more likely to relapse if they were abstinent at 18 months than if they were drinking without problems, even if they were highly alcohol-dependent (Table 3). Thus the Rand study found a strong link between severity and outcome, but a far from ironclad one.
Some studies have failed to confirm the link between controlled-drinking versus abstinence outcomes and alcoholic severity. In a clinical trial that included CD and abstinence training for a highly dependent alcoholic population, Rychtarik et al. (1987) reported 18 percent controlled drinkers and 20 percent abstinent (from 59 initial patients) at 5 to 6 year follow-up. Outcome type was not related to severity of dependence. Nor was it for Nordström and Berglund (1987), perhaps because they excluded "subjects who were never alcohol dependent."
Nordström and Berglund, like Wallace et al. (1988), selected high-prognosis patients who were socially stable. The Wallace et al. patients had a high level of abstinence; patients in Nordström and Berglund had a high level of controlled drinking. Social stability at intake was negatively related in Rychtarik et al. to consumption as a result either of abstinence or of limited intake. Apparently, social stability predicts that alcoholics will succeed better whether they choose abstinence or reduced drinking. But other research indicates that the pool of those who achieve remission can be expanded by having broader treatment goals.
Rychtarik et al. found that treatment aimed at abstinence or controlled drinking was not related to patients' ultimate remission type. Booth, Dale, and Ansari (1984), on the other hand, found that patients did achieve their selected goal of abstinence or controlled drinking more often. Three British groups (Elal-Lawrence, Slade, & Dewey, 1986; Heather, Rollnick, & Winton, 1983; Orford & Keddie, 1986) have found that treated alcoholics' beliefs about whether they could control their drinking and their commitment to a CD or an abstinence-treatment goal were more important in determining CD versus abstinence outcomes than were subjects' levels of alcohol dependence. Miller et al. (in press) found that more dependent drinkers were less likely to achieve CD outcomes but that desired treatment goal and whether one labeled oneself an alcoholic or not independently predicted outcome type.
Summary
Controlled drinking has an important role to play in alcoholism treatment. Controlled drinking as well as abstinence is an appropriate goal for the majority of problem drinkers who are not alcohol-dependent. In addition, while controlled drinking becomes less likely the more severe the degree of alcoholism, other factors—such as age, values, and beliefs about oneself, one's drinking, and the possibility of controlled drinking—also play a role, sometimes the dominant role, in determining successful outcome type. Finally, reduced drinking is often the focus of a harm-reduction approach, where the likely alternative is not abstinence but continued alcoholism.
(SEE ALSO: Alcohol; Disease Concept of Alcoholism and Drug Abuse; Relapse Prevention; Treatment)
Table 1. Selected Alcoholism Outcome Studies
| Study |
Years of
Follow-up |
No. of
Assessed
Subjects |
Percent
Abstinent |
Percent
Controlled
Drinking |
Percent
Remission
Survivors (a) |
| Untreated |
|
|
|
|
|
| Goodwin, Crane, & Guze (1971) |
8 |
93 |
8 |
33 (b) |
41 |
| 1989 Canadian National Survey |
>=1 |
497 |
49 |
51 |
100 (c) |
| |
|
|
|
|
|
| Treated |
|
|
|
|
|
| Rand (Polich, Armor, & Braiker 1981) |
4 |
548 |
28 |
18 (d) |
46 |
| Vaillant (1983) |
8 |
100 |
39 |
6 |
45 |
| Helzer et al. (1985) (e) |
5-7 |
387 |
15 (f) |
18 (g) |
33 |
| McCabe (1986) |
16 |
31 |
26 |
35 |
61 |
| Nordström & Berglund (1987) |
18-24 |
55 |
20 |
38 |
58 |
| Rychtarik et al. (1987) |
5-6 |
43 |
23 |
21 |
44 |
| Wallace et al. (1988) |
0.5 |
169 |
68 (h) |
-(h) |
68 (h) |
| Finney and Moos (1991) |
10 |
83 |
54 |
24 |
78 |
| Walsh et al. (1991) |
2 |
200 |
23 (37) (i) |
10 (7) (i) |
33 (44) (i) |
|
|
Table 2. Controlled Drinking and Abstinence in Relation to Treated and Untreated Remission: The 1989 Canadian National Alcohol and Drug Survey
(Data Weighted to Represent National Population)
| |
Treated Remission (n = 89) |
Untreated Remission (n = 408) |
| Abstinent (51%) |
92 |
39 |
| Nonabstinent (49%) |
8 |
61 |
|
|
Table 3. Relapse Rates at 4-Year Follow-up According to Remission Category at Eighteen Months, by Alcohol Dependence Category, Marital Status, and Age
| |
Age < 40 at Admission |
Age > 40 at Admission |
| |
Abstaining
18 Months |
Nonproblem
Drinking
18 Months |
Abstaining
18 Months |
Nonproblem
Drinking
18 Months |
High Dependence Symptoms
Married |
12 |
17 |
14 |
50 |
| Single |
21 |
7 |
24 |
28 |
Low Dependence Symptoms
Married |
16 |
7 |
19 |
28 |
| Single |
29 |
3 |
32 |
13 |
|
|
next: A Moral Vision of Addiction
~ all Stanton Peele articles
~ addictions library articles
~ all addictions articles
Bibliography
BOOTH, P. G., DALE, B., & ANSARI, J. (1984). Problem drinkers' goal choice and treatment outcomes: A preliminary study. Addictive Behaviors, 9, 357-364.
EDWARDS, G., ET AL. (1983). What happens to alcoholics? Lancet, 2, 269-271.
ELAL-LAWRENCE, G., SLADE, P. D., & DEWEY, M. E. (1986). Predictors of outcome type in treated problem drinkers. Journal of Studies on Alcohol, 47, 41-47.
FINNEY, J. W., & MOOS, R. H. (1991). The long-term course of treated alcoholism: 1. Mortality, relapse and remission rates and comparisons with community controls. Journal of Studies on Alcohol, 52, 44-54.
GOODWIN, D. W., CRANE, J. B., & GUZE, S. B. (1971). Felons who drink: An 8-year follow-up. Quarterly Journal of Studies on Alcohol, 32, 136-47.
HEATHER, N. (1992). The application of harm-reduction principles to the treatment of alcohol problems. Paper presented at the Third International Conference on the Reduction of Drug-Related Harm. Melbourne Australia, March.
HEATHER, N., ROLLNICK, S., & WINTON, M. (1983). A comparison of objective and subjective measures of alcohol dependence as predictors of relapse following treatment. Journal of Clinical Psychology, 22, 11-17.
HELZER, J. E. ET AL., (1985). The extent of long-term moderate drinking among alcoholics discharged from medical and psychiatric treatment facilities. New England Journal of Medicine, 312, 1678-1682.
HYMAN, H. H. (1976). Alcoholics 15 years later. Annals of the New York Academy of Science, 273, 613-622.
McCABE, R. J. R. (1986). Alcohol-dependent individuals 16 years on. Alcohol & Alcoholism, 21, 85-91.
MILLER, W. R. ET AL., (1992). Long-term follow-up of behavioral self-control training. Journal of Studies on Alcohol, 53, 249-261.
NORDSTRÖM, G., & BERGLUND, M. (1987). A prospective study of successful long-term adjustment in alcohol dependence. Journal of Studies on Alcohol, 48, 95-103.
ORFORD, J., & KEDDIE, A. (1986). Abstinence or controlled drinking: A test of the dependence and persuasion hypotheses. British Journal of Addiction, 81, 495-504.
PEELE, S. (1992). Alcoholism, politics, and bureaucracy: The consensus against controlled-drinking therapy in America. Addictive Behaviors, 17, 49-61.
PEELE, S. (1987). Why do controlled-drinking outcomes vary by country, era, and investigator?: Cultural conceptions of relapse and remission in alcoholism. Drug and Alcohol Dependence, 20, 173-201.
POLICH, J. M., ARMOR, D. J., & BRAIKER, H. B. (1981). The course of alcoholism: Four years after treatment. New York: Wiley.
ROSENBERG, H. (1993). Prediction of controlled drinking by alcoholics and problem drinkers. Psychological Bulletin, 113, 129-139.
ROSENBERG, H., MELVILLE, J., LEVELL., D., & HODGE, J. E. (1992). A ten-year follow-up survey of acceptability of controlled drinking in Britain. Journal of Studies on Alcohol, 53, 441-446.
RYCHTARIK, R. G., ET Al., (1987). Five-six-year follow-up of broad spectrum behavioral treatment for alcoholism: Effects of training controlled drinking skills. Journal of Consulting and Clinical Psychology, 55, 106-108.
SKINNER, H. A. (1990). Spectrum of drinkers and intervention opportunities. Journal of the Canadian Medical Association, 143, 1054-1059.
VAILLANT, G. E. (1983). The natural history of alcoholism. Cambridge: Harvard University Press.
WALLACE, J., ET AL., (1988). 1. Six-month treatment outcomes in socially stable alcoholics: Abstinence rates. Journal of Substance Abuse Treatment, 5, 247-252.
WALSH, D. C., ET AL., (1991). A randomized trial of treatment options for alcohol-abusing workers. New England Journal of Medicine, 325, 775-782.

 The usual dose is 2 milligrams to 10 milligrams 3 or 4 times daily.
The usual dose is 2 milligrams to 10 milligrams 3 or 4 times daily. I'm doing well on the OCD front except for when that voice creeps up on me and whispers uncertainty into my ear. Actually, because of the cold I think my resistance to it isn't as strong as it should be and the floor defiantly still feels dodgy to me. However, my determination is staying strong. As you know, I'm staying at my friends house and it seems like I shall be for a little while... Hubby is at a low point and needs a break from the OCD. He keeps catching colds and is feeling very down at the moment. I guess doing so much for me over the years has taken it's toll on him too, and he feels mentally exhausted, plus I think he's scared of me returning to how I was OCD-wise at home. Now that he's seen what I can live like here he doesn't want that for me. We're seeing each other every week though, and talk everyday.
I'm doing well on the OCD front except for when that voice creeps up on me and whispers uncertainty into my ear. Actually, because of the cold I think my resistance to it isn't as strong as it should be and the floor defiantly still feels dodgy to me. However, my determination is staying strong. As you know, I'm staying at my friends house and it seems like I shall be for a little while... Hubby is at a low point and needs a break from the OCD. He keeps catching colds and is feeling very down at the moment. I guess doing so much for me over the years has taken it's toll on him too, and he feels mentally exhausted, plus I think he's scared of me returning to how I was OCD-wise at home. Now that he's seen what I can live like here he doesn't want that for me. We're seeing each other every week though, and talk everyday.

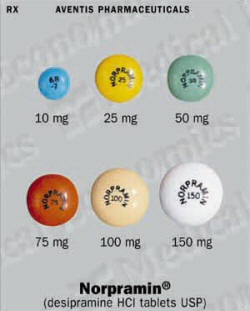 Pregnant women or mothers who are nursing an infant should use Norpramin only when the potential benefits clearly outweigh the potential risks. If you are pregnant or planning to become pregnant, inform your doctor immediately.
Pregnant women or mothers who are nursing an infant should use Norpramin only when the potential benefits clearly outweigh the potential risks. If you are pregnant or planning to become pregnant, inform your doctor immediately.